Opiate Sparing Interventional Pain Live Workshops and Online CME Courses
Case Study 1
59 year old male with amputation above the knee on his left side presents with chronic stump and phantom limb pain. Patient is currently taking oxycodone 5 mg to six hours PRN. Patient reports medication is not effectively alleviate his pain and his failed non-opiate medication therapy such as gabapentin and Aleve. Patient was never offered airbox or interventional pain procedures to alleviate his pain. After undergoing Femoral nerve injection, 90% of his pain is relieved. Patient that undergoes peripheral nerve stimulator trial at the femoral nerve under ultrasound guidance. Patient reports nearly 100% pain relief after 20 minutes of femoral nerve stimulation. Patient goes on to have a stimrouter peripheral nerve stimulator place to alleviate his pain. Patient is currently three years post implantation and is pain-free when utilizing the device to alleviate his pain. He is now free of opiates and able to travel the world and visit family in the Dominican Republic.
90% of his pain is relieved. Patient that undergoes peripheral nerve stimulator trial at the femoral nerve under ultrasound guidance. Patient reports nearly 100% pain relief after 20 minutes of femoral nerve stimulation. Patient goes on to have a stimrouter peripheral nerve stimulator place to alleviate his pain. Patient is currently three years post implantation and is pain-free when utilizing the device to alleviate his pain. He is now free of opiates and able to travel the world and visit family in the Dominican Republic.
 90% of his pain is relieved. Patient that undergoes peripheral nerve stimulator trial at the femoral nerve under ultrasound guidance. Patient reports nearly 100% pain relief after 20 minutes of femoral nerve stimulation. Patient goes on to have a stimrouter peripheral nerve stimulator place to alleviate his pain. Patient is currently three years post implantation and is pain-free when utilizing the device to alleviate his pain. He is now free of opiates and able to travel the world and visit family in the Dominican Republic.
90% of his pain is relieved. Patient that undergoes peripheral nerve stimulator trial at the femoral nerve under ultrasound guidance. Patient reports nearly 100% pain relief after 20 minutes of femoral nerve stimulation. Patient goes on to have a stimrouter peripheral nerve stimulator place to alleviate his pain. Patient is currently three years post implantation and is pain-free when utilizing the device to alleviate his pain. He is now free of opiates and able to travel the world and visit family in the Dominican Republic.Case Study 2
39-year-old female presents with a chronic history of neuralgia paresthetica. She has tried neuropathic pain medication, physical therapy, weight loss and neuropathic pain medication such as gabapentin and pre-Gabalin without relief. Patient undergoes diagnostic nerve block under ultrasound at the lateral femoral cutaneous nerve which alleviate all for symptoms for 1 day, but her symptoms slowly return.
Patient agreed to cryo- Ablative therapy and undergoes office based ultrasound guided cryo- ablation of the lateral femoral cutaneous nerve. The procedure gives her nearly complete relief for three months. That’s a three month mark the mileage cells which cover the axons of the nerves grow back and the nurse starts to function as he did previously. Pain baseline is that a lower level and patient returns for repeat lesioning. Patient is currently able to function normally between interventions and is not dependent on opiates.
Case Study 3
68 year old veteran presents to the emergency room with exacerbation of radicular pain. Patient has a history of prior discectomy and is currently taking Lyrica for his chronic radicular pain. Patient usually gets by fairly well and occasionally uses Percocet to manage his pain. Pain exacerbated while lifting a heavy box and is currently incapacitating 10/10 right side radiating pain. Upon presenting to the emergency room, patient has straight leg raise and presents with obvious clinical radiculopathy. After ruling out infection, nerve deficits, or more serious pathology, the emergency room physician who is trained in ultrasound agrees to perform an ultrasound guided caudal epidural steroid injection with steroid and saline. The patient receives the injection and is subsequently discharged as his pain score drops from 10 out of 10 to 4 out of 10 immediately after saline and steroid injection. The patient then referred to the Pain Management office for follow up.
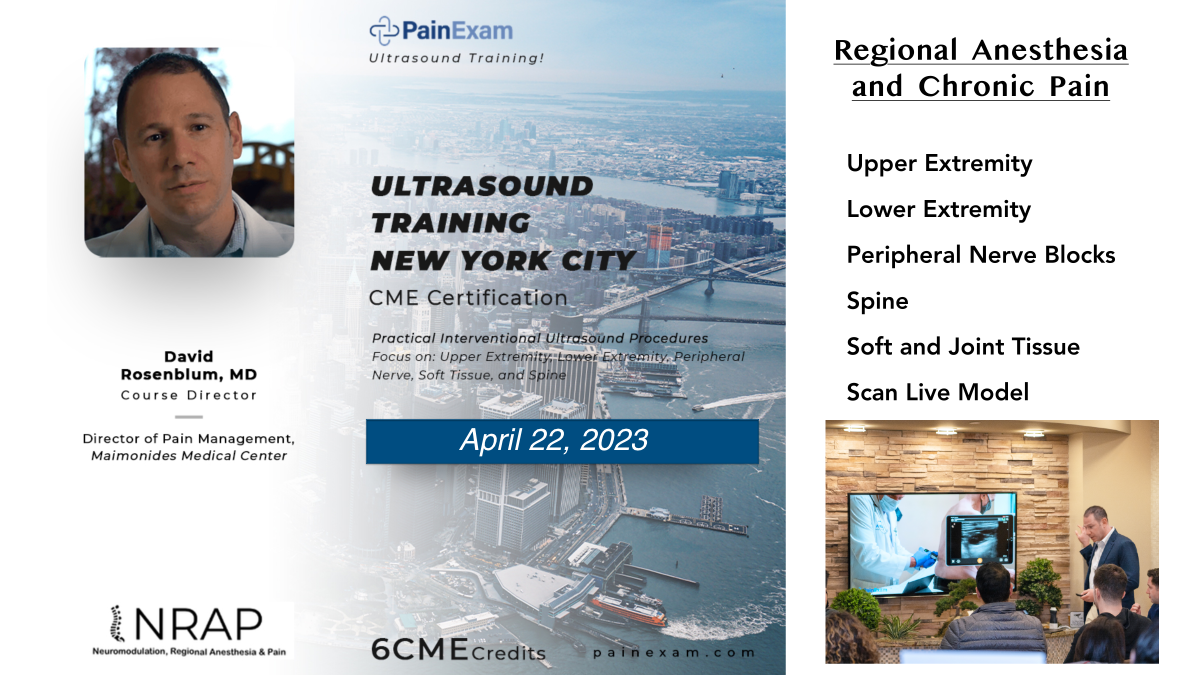
Clinicians who come to our workshops and courses. come from various backgrounds. They are not all interventional pain physicians, trained in PM&R or Anesthesiology. Many come from the emergency room, family medicine, orthopedics, radiology or are APPs.
Our program offer something for everyone and we believe in cost-effective safe and practical pain medicine. NRAP encourages respect for the scope of practice and limitation that are placed upon practitioners should be respected, however, with new technologies, situations and availabilities of therapy, we encourage the expansion of practice scopes to minimize opiate dispensing and provide accessible care. It is simply not acceptable to have a patient spend a full week in the hospital to wait for an epidural steroid injection or to get put on excessively high hope your vacations to alleviate the pain.
Check out our Calendar below and Subscribe to our Newsletter